Parkinson's disease stands as one of the world's fastest-growing neurological conditions, affecting an estimated 1.1 million people in the United States and 166,000 in the United Kingdom today. Yet despite its prevalence, many people misunderstand what the disease actually is—and more importantly, what living with it can look like. This comprehensive guide breaks down everything you need to know about Parkinson's, from the science behind it to cutting-edge treatments and practical strategies for managing symptoms.
What Exactly Is Parkinson's Disease?
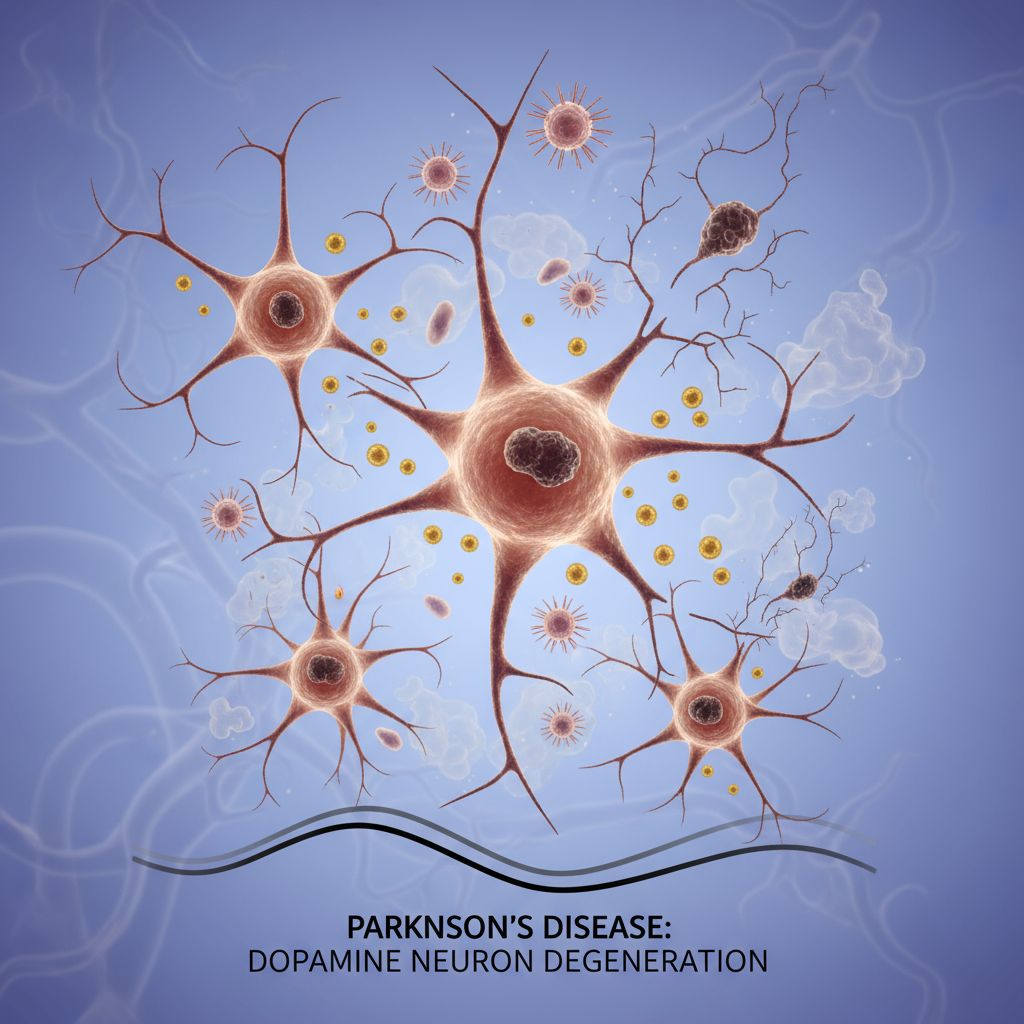
Parkinson's disease is a progressive neurodegenerative disorder that primarily affects your nervous system, causing both movement and non-movement problems that worsen over time. The condition develops when nerve cells in a specific brain region called the substantia nigra—responsible for producing dopamine—gradually break down or die.
Dopamine is a chemical messenger that your brain uses to control smooth, purposeful movement. When these cells die, your brain can't send proper signals to your muscles, resulting in the hallmark symptoms of tremors, stiffness, and slowness. The truly striking aspect: by the time symptoms appear, most people have already lost between 60 to 80% of their dopamine-producing neurons. This is why early detection matters so much—catching the disease before extensive neurological damage can make a real difference in treatment outcomes.
The Brain Behind the Disease
When researchers examine the brains of people with Parkinson's, they find distinctive clumps of proteins called Lewy bodies, composed mainly of a protein called alpha-synuclein. Scientists believe these protein accumulations trigger a cascade of cellular damage. The body's protein disposal system appears to fail in Parkinson's patients, allowing proteins to build up to harmful levels and trigger the death of neurons. This discovery has become central to developing new treatments that target this specific mechanism.
Motor Symptoms: What You Actually Experience
The movement problems associated with Parkinson's develop gradually, often starting so subtly that you might not notice them immediately. The classic triad of Parkinson's symptoms includes tremor, rigidity, and bradykinesia—medical speak for slow movement.
Tremors typically begin as a slight shake in one hand at rest and can eventually spread. Unlike other types of shaking, Parkinson's tremors often diminish or disappear when you actively use your hands. Muscle rigidity creates that distinctive stiffness and resistance to movement, making everyday tasks feel laborious. Slowness of movement can make simple activities like buttoning a shirt or getting out of bed feel exhaustingly time-consuming.

Additional motor complications emerge as the disease progresses, including balance problems, difficulties walking (sometimes with a characteristic shuffling gait), changes to your posture, and slowed or quiet speech. Some people develop micrographia—handwriting that becomes progressively smaller and harder to read. These symptoms don't just create inconvenience; they significantly impact quality of life and independence.
Beyond Movement: Non-Motor Symptoms That Matter
What catches many people off guard is that Parkinson's extends far beyond shaky hands. Non-motor symptoms can be just as challenging as movement problems, sometimes appearing before motor symptoms even develop.
Sleep disturbances rank among the most common non-motor issues, with people experiencing everything from insomnia to vivid dreams and acting out dream content. Depression and anxiety frequently accompany the disease, affecting roughly 30-40% of patients. Cognitive changes range from mild slowing of thoughts to dementia-like symptoms in advanced stages, affecting up to 50% of people in stages 4 and 5. Other non-motor symptoms include decreased sense of smell, constipation, low blood pressure (especially when standing), fatigue that rest doesn't relieve, and swallowing difficulties.
The loss of norepinephrine—another crucial neurotransmitter—explains many of these non-motor symptoms. This dual neurotransmitter loss creates a complex symptom profile that requires comprehensive treatment approaches.
The Five Stages: Understanding Disease Progression
Parkinson's follows a generally predictable pattern, though progression speed varies dramatically between individuals. Understanding these stages helps you anticipate changes and plan accordingly.
Stage 1: Subtle Beginnings
Mild symptoms appear that don't significantly interfere with daily life. Tremors or stiffness typically affect only one side of the body. Family members might notice subtle changes in movement or posture. Many people continue their normal routines with minimal adjustment.
Stage 2: Moderate Progression
Symptoms become noticeably more pronounced, affecting both sides of the body (though often asymmetrically). Muscle stiffness and rigidity can slow task completion. Posture changes may develop, and speech might become quieter. People can still live independently but find certain activities more challenging.
Stage 3: The Turning Point
This middle stage marks a significant shift. Balance and reflexes deteriorate, movements slow considerably, and falls become more common. However, people can still complete daily tasks with more effort and time. Physical therapy becomes increasingly valuable.
Stage 4: Advanced Limitations
Independence becomes severely compromised. While standing without assistance may still be possible, movement typically requires assistive devices like walkers. Living alone becomes dangerous and impractical. Confusion, hallucinations, and delusions affect roughly half of people at this stage.
Stage 5: Severe Dependence
The most advanced stage requires full-time care. People typically need wheelchairs and cannot stand or walk without falling. Advanced leg stiffness can cause freezing. Cognitive and psychiatric symptoms often intensify.
Progression timeframes vary wildly—some people spend years in each stage, while others advance more rapidly. Importantly, the stage someone reaches isn't predetermined by age or initial symptoms.
What Causes Parkinson's? Genes, Environment, and Mystery
Despite decades of research, scientists still don't fully understand why Parkinson's develops. However, they've identified multiple contributing factors that likely work together.
Genetic Factors
Specific genetic mutations increase Parkinson's risk, though genetic cases represent only about 10-15% of all cases. Having a close family member with Parkinson's increases your risk, but these genetic links are relatively rare unless multiple family members have the disease.
Environmental Influences
Exposure to certain toxins appears to increase risk. Pesticides, well water, solvents, and air pollution all show associations with increased Parkinson's development. A controversial substance called MPTP, sometimes sold illegally as "synthetic heroin," can rapidly cause Parkinson's-like symptoms.
A Surprising Discovery: Viral Connection
Recent groundbreaking research from Northwestern Medicine discovered that a usually harmless virus called human pegivirus (HPgV) may play a role. Scientists found HPgV in the brains and spinal fluid of Parkinson's patients but not in healthy controls. Patients with the virus showed more advanced brain changes, including increased tau pathology. This viral trigger may interact with genetic factors, creating a two-hit model of disease development.
Age and Other Factors
Age remains the most significant risk factor, with most diagnoses occurring after age 60, though one in ten diagnosed patients are under 45 years old. Men develop Parkinson's more frequently than women, though scientists aren't certain why.
Diagnosis: From Symptoms to Confirmation
Here's the frustrating reality: there's no definitive test that conclusively diagnoses Parkinson's disease. Doctors primarily diagnose based on clinical symptoms, physical examination, and neurological testing—sometimes after significant neurological damage has already occurred.
Neurologists look for the classic motor symptoms—tremor, rigidity, slowness, and balance problems—and test your reflexes and coordination. They may order imaging studies like MRI or PET scans to rule out other conditions.
Blood Tests: The Future of Early Detection
This is where recent breakthroughs become genuinely exciting. Researchers have developed multiple blood-based tests that could revolutionize early detection:
Alpha-Synuclein Seed Amplification Assay (α-syn SAA)
This breakthrough test detects misfolded alpha-synuclein proteins in blood samples. Remarkably, it can identify Parkinson's disease up to 10 years before clinical symptoms appear. In studies, the test was 100% accurate in people with diagnosed Parkinson's, and positive in 30% of people with REM sleep behavior disorder—a condition that frequently precedes Parkinson's. The test achieved 87.7% accuracy in identifying people with Parkinson's disease in a large 2023 study.
RNA-Based Tests
In April 2025, researchers at Hebrew University unveiled an RNA-based blood test measuring specific transfer RNA fragments (tRFs) that can detect Parkinson's years before symptoms emerge. The test shows promise for scalability and affordability, potentially offering accessibility to routine screening.
Protein Panels
Other researchers identified eight blood proteins associated with Parkinson's disease severity that together can help identify people at risk or in early stages.
While none of these tests are yet approved for routine clinical diagnosis, they represent a seismic shift in the field. Soon, people might receive Parkinson's diagnoses before ever experiencing tremors—opening windows for early intervention when treatments might prove most effective.
Current Treatments: Managing Symptoms Effectively
While there's still no cure for Parkinson's disease, multiple treatment approaches can significantly improve quality of life and manage symptoms, particularly if started early.
Medications: The Dopamine Approach
Levodopa remains the gold standard medication for Parkinson's. This medication is converted into dopamine in your brain, replenishing depleted supplies. It's usually combined with other medications like carbidopa or benserazide that prevent breakdown in the bloodstream and reduce side effects. Most people eventually need levodopa, and initial doses are small, gradually increased until symptoms improve.
The downside: as more dopamine neurons die, levodopa becomes progressively less effective. Long-term use can cause involuntary jerky movements (dyskinesias) and "on-off" effects, where people rapidly switch between being able to move and becoming immobilized.
Dopamine Agonists
These medications mimic dopamine's effects without being converted to dopamine itself. Examples include pramipexole, ropinirole, and rotigotine.
Monoamine Oxidase-B Inhibitors
Medications like selegiline and rasagiline prevent dopamine breakdown, extending its availability in the brain.
Your neurologist will determine which medications work best for your specific situation, as individual responses vary significantly.

Surgical Interventions: Cutting-Edge Options
Deep Brain Stimulation (DBS)
DBS involves surgically implanting electrodes that deliver electrical pulses to specific brain regions, effectively suppressing symptoms. In 2025, the FDA approved adaptive DBS, a closed-loop system that automatically adjusts stimulation in real-time based on brain activity—a major advancement. Previously, adjustments required visiting a clinician.
Focused Ultrasound (FUS)
This newer approach uses targeted ultrasound waves to create small lesions in specific brain areas, improving symptoms. In 2025, FDA approval extended FUS to treat both sides of the brain through separate procedures, offering new possibilities for broader symptom relief.
Stem Cell Therapy: Hope on the Horizon
Two exciting clinical trials published in Nature in April 2025 demonstrated that injecting stem-cell-derived dopamine neurons into the brain is safe. Some participants experienced visible tremor reduction, and the transplanted cells survived and continued producing dopamine. While these early trials involved only 19 people and were primarily designed to test safety, they represent "a big leap in the field," according to stem-cell biologist Malin Parmar. Larger trials are underway to determine effectiveness.
Breakthrough Treatments in Development
The most exciting news involves disease-modifying therapies—treatments that might actually slow or stop disease progression, not just manage symptoms.
Prasinezumab: A Game-Changer
In June 2025, Swiss pharmaceutical company Roche announced that prasinezumab is advancing into Phase III clinical trials, the critical stage before potential FDA approval. This drug targets toxic alpha-synuclein buildup, potentially binding to harmful proteins and limiting their damage to dopamine neurons. If successful, prasinezumab could become among the first disease-modifying medications available to the public.
World's Largest Clinical Trial Underway
In October 2025, researchers at UCL and Newcastle University launched the world's largest-ever Parkinson's disease trial—a £26 million project recruiting up to 1,600 participants from more than 40 hospitals across the UK. Using an innovative flexible design that tests multiple treatments in parallel, the trial could reduce drug testing timelines by up to three years. Participants are already being recruited, with most trial sites launching between now and April 2026.
These developments represent a genuine inflection point. For the first time, we're not just managing symptoms—we're pursuing treatments that could fundamentally alter disease progression.
Living Well: Lifestyle Strategies That Work
While medication and surgery treat symptoms, lifestyle modifications can profoundly impact how you experience Parkinson's. Research consistently shows that comprehensive lifestyle approaches produce better outcomes than medication alone.
Exercise: The Most Powerful Tool
Regular physical activity ranks among the most effective interventions for Parkinson's disease. Exercise improves balance, preserves mobility, maintains muscle strength, and enhances mood. Starting exercise early in disease progression helps you maintain quality of life long-term.
Yoga and Pilates
Yoga improves walking ability, reduces tremors, enhances flexibility, and corrects posture—all while reducing anxiety. Pilates focuses more on strength-building while also improving coordination and balance through low-impact movements.
Dance Therapy
If structured exercise sounds boring, dance therapy offers a fun alternative. Working with a dance therapist gets your whole body moving, improving coordination and balance while providing social connection and emotional support.
Strength Training
Weight training builds endurance and muscle strength, crucial components of balance and mobility.
Walking and Aerobic Exercise
Regular aerobic activity, including simple walking, preserves cardiovascular health and supports overall functioning.
Frequently Asked Questions
Nutrition: Fueling Your Brain
A predominantly whole-food, plant-based diet rich in antioxidants supports brain health. Fresh produce, whole grains, lean proteins, and adequate hydration form the foundation.
Fiber-Rich Foods
Whole grains like millets and brown rice, pulses, and fresh vegetables combat constipation—a common Parkinson's problem—and stabilize blood sugar.
Strategic Protein Timing
Protein can interfere with levodopa absorption. Time protein intake away from dopaminergic medications to optimize medication effectiveness, but don't eliminate protein—your body needs it.
Antioxidant Powerhouses
Traditional spices like turmeric, ginger, and garlic; nuts; fresh fruits; and green tea support neural health and reduce inflammation.
Bone Health Support
Vitamin D and calcium become increasingly important as falls become a risk. Dairy products, eggs, and fortified cereals provide these crucial nutrients.
Sleep: The Overlooked Essential
Parkinson's frequently disrupts sleep, but establishing consistent sleep routines and creating a relaxing sleep environment can help. If sleep problems persist, discuss options with your doctor—managing sleep often improves daytime symptoms and mood.
Stress Management and Mental Health
Stress can worsen Parkinson's symptoms significantly. Relaxation techniques, deep breathing exercises, and mindfulness meditation help manage stress while supporting overall well-being. Don't overlook depression and anxiety—these respond well to treatment and shouldn't be accepted as inevitable parts of Parkinson's.
Social Connection and Mental Stimulation
Staying socially connected and mentally active protects against isolation and cognitive decline. Puzzles, reading, learning new skills, and meaningful social interaction all support brain health and emotional well-being.
Support Groups: You're Not Alone
Connecting with others who have Parkinson's through support groups provides emotional support, practical strategies, and the comfort of knowing you're not alone in this journey.
The Road Ahead
Parkinson's disease remains a complex challenge without a cure—but the landscape is changing rapidly. Blood tests might soon detect the disease a decade before symptoms appear. Disease-modifying therapies moving through clinical trials could fundamentally alter disease progression. Adaptive surgical interventions offer personalized symptom management. Stem cell research shows genuine promise.
Most importantly, we understand more than ever before that living well with Parkinson's isn't about a single treatment—it's about integrating medication, physical therapy, lifestyle modifications, psychological support, and social connection into a comprehensive approach tailored to each person's needs.
If you suspect you might have Parkinson's disease—whether due to tremors, slowness, balance problems, or non-motor symptoms like lost sense of smell or sleep disturbances—talk to your healthcare provider. Early evaluation matters. And if you've recently received a diagnosis, know that your life isn't over; it's simply entering a new chapter where proactive management and lifestyle choices genuinely matter.
The future of Parkinson's disease treatment has never looked brighter.