The year 2025 has emerged as a transformative period in cancer treatment, with groundbreaking innovations that are fundamentally changing how we approach this devastating disease. From ultrasound-controlled immune cells to universal mRNA vaccines, these revolutionary therapies are offering hope to millions of patients worldwide while dramatically reducing the need for invasive surgical procedures.
The Immunotherapy Revolution: 80% of Patients May Skip Surgery
One of the most remarkable breakthroughs reported in 2025 involves immunotherapy treatments that could eliminate the need for surgery in 80% of patients with specific genetic mutations. A groundbreaking study published in the New England Journal of Medicine revealed that patients with tumors containing mismatch repair deficiency—a genetic mutation affecting colorectal, gastric, pancreatic, and endometrial cancers—responded exceptionally well to immunotherapy alone.
The treatment works by exposing tumors to the immune system rather than simply boosting immune responses. As researchers explain, when the immune system recognizes these genetically defective tumors as foreign, it can completely eliminate them from the body. This approach has proven 80% effective in patients with the specific mutation, representing a paradigm shift from traditional surgical interventions.
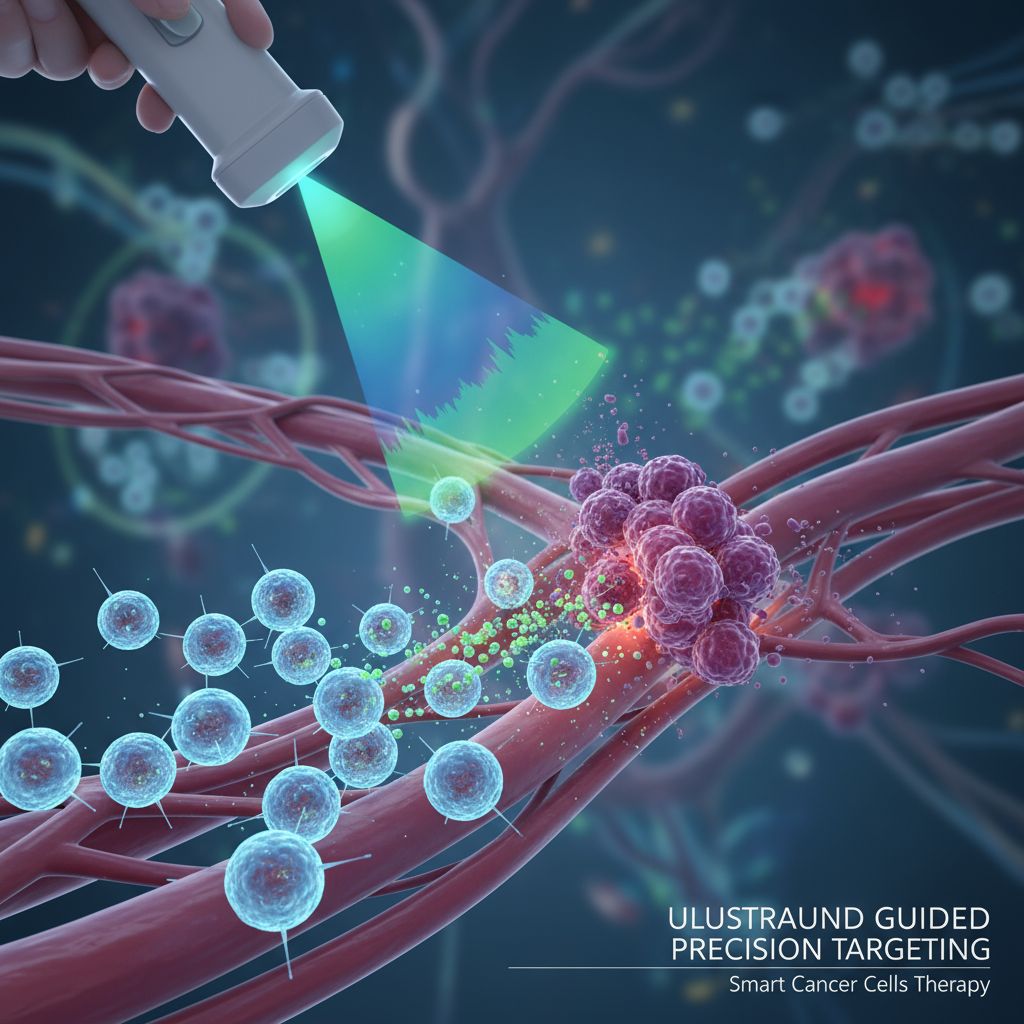
Smart CAR-T Cells: The Five-Day Cancer Fighters
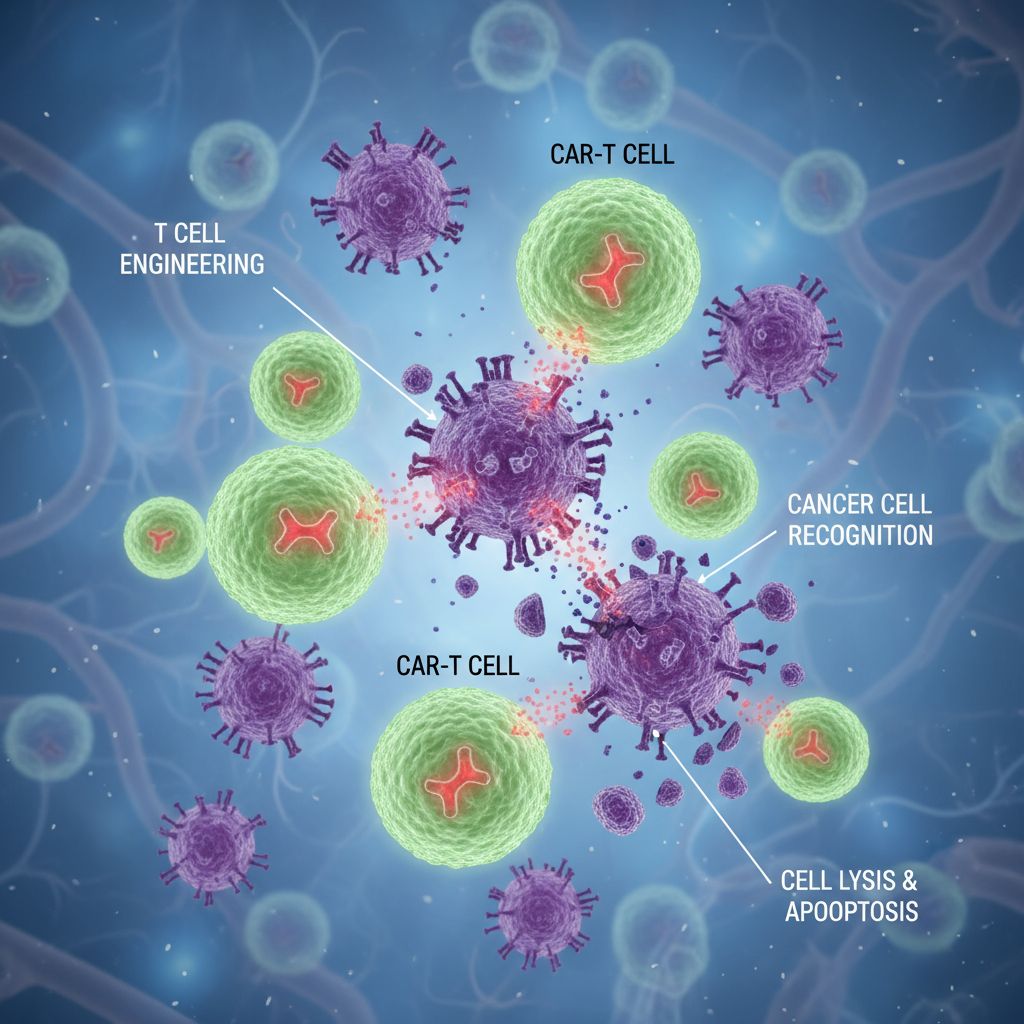
EchoBack CAR-T Cells: Precision Meets Longevity
USC researchers have developed revolutionary "EchoBack CAR-T cells" that represent a quantum leap in cancer immunotherapy. Unlike traditional CAR-T cells that typically function for only 24 hours, these smart immune cells can continuously attack cancer cells for at least five days without becoming exhausted.
The breakthrough lies in their ultrasound-controlled activation system. These engineered cells can be remotely activated using focused ultrasound pulses lasting just 10 minutes, triggering them to seek and destroy cancer cells in their immediate vicinity. The cells are designed with a unique "call-and-response" mechanism—whenever a tumor cell is nearby, it sends signals to the CAR-T cells, which then produce more killing molecules to eliminate the threat.
Safety Through Smart Design
What makes EchoBack CAR-T cells particularly revolutionary is their built-in safety mechanism. When these cells migrate away from tumor sites, the CAR molecules gradually degrade, ensuring they won't attack healthy tissue. This smart design addresses one of the major concerns with traditional CAR-T therapy: on-target, off-tumor toxicity.
Laboratory results have been stunning. In mouse models testing prostate cancer and glioblastoma, ultrasound-controllable CAR-T cells significantly outperformed standard CAR-T cells, showing enhanced killing ability and reduced exhaustion even when repeatedly challenged with tumor cells.
Universal mRNA Cancer Vaccines: The Holy Grail of Oncology
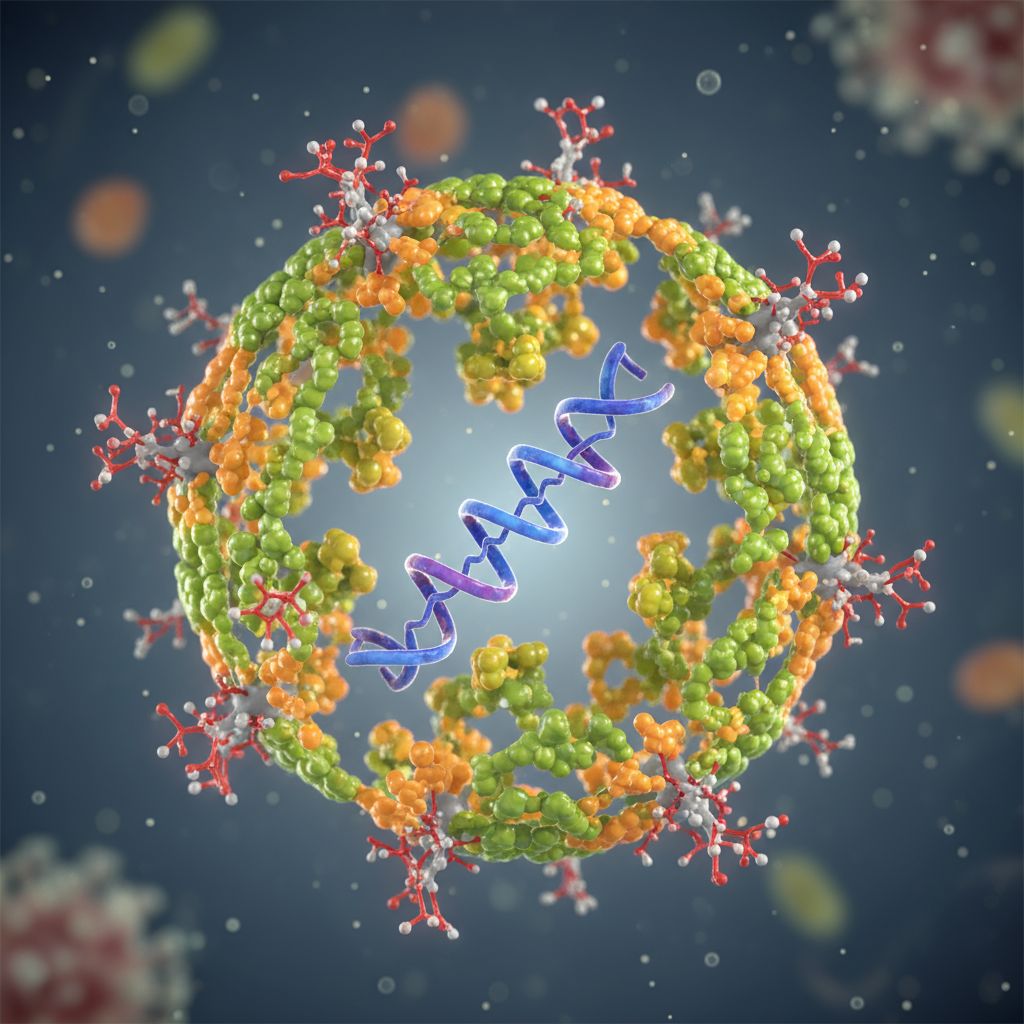
Breaking the Specificity Barrier
University of Florida researchers have achieved what many considered impossible: developing a universal mRNA cancer vaccine that doesn't target specific tumor proteins but instead revs up the entire immune system. This groundbreaking approach works by stimulating the expression of PD-L1 protein inside tumors, making them more receptive to treatment.
Unlike traditional cancer vaccines that require identification of specific targets or personalized approaches, this universal vaccine generates broad anti-cancer immunity by essentially tricking the immune system into responding as if fighting a virus. When combined with immune checkpoint inhibitors, the results have been dramatic—tumors shrunk significantly, and in some cases, the vaccine alone completely eliminated tumors.
Clinical Promise and Future Applications
The research, published in Nature Biomedical Engineering, represents a potential alternative to surgery, radiation, and chemotherapy with broad implications for treating resistant tumors. The vaccine's ability to activate previously non-functional T cells and multiply their anti-cancer response suggests it could work across multiple cancer types.
Personalized Cancer Vaccines: Tailored Medicine Goes Global
AI-Powered Precision Medicine
Russia's Gamaleya Center has commenced human trials for a personalized mRNA melanoma vaccine developed using artificial intelligence algorithms. The entire process—from tumor sequencing to vaccine production—can be completed within one week, representing a significant acceleration compared to typical personalized therapy timelines.
This vaccine differs fundamentally from COVID-19 mRNA vaccines by encoding multiple neoantigens specific to each patient's tumor, offering a multi-targeted immune approach that addresses both primary tumors and metastatic sites. The Russian government plans to provide this treatment free of charge to citizens, with production costs around $2,869 per dose.
Advanced Clinical Results
The NeoVax MI personalized cancer vaccine has shown remarkable improvements in immune response compared to previous formulations. Dana-Farber Cancer Institute's phase 1 trial demonstrated that changes in formulation and administration significantly enhanced the vaccine's immunogenicity. Meanwhile, EVX-01, an AI-designed personalized vaccine, achieved a 67% objective response rate in metastatic melanoma patients, with two complete and six partial responses out of twelve patients.
Extracellular Vesicles: Nature's Precision Delivery System
Microscopic Medical Couriers
Scientists at Kanazawa University have developed antigen-presenting extracellular vesicles (AP-EVs) that represent a breakthrough in targeted cancer therapy. These tiny, naturally occurring particles boost the immune system to fight tumors more effectively while reducing harmful side effects.
Unlike traditional immunotherapy that can cause broad immune activation and unwanted effects, AP-EVs provide precise targeting of tumor-fighting T cells, leading to tumor eradication without harming healthy tissue. Advanced imaging techniques have confirmed that these vesicles accumulate specifically in tumors, making them ideal for targeted therapy.
Cutting-Edge Technologies Reshaping Treatment
Light-Based Therapy Precision
New light-based cancer therapies are achieving remarkable results with minimal side effects. Recent developments in photodynamic therapy have shown the ability to kill 92% of skin cancer cells without harming healthy tissue. This approach uses specific wavelengths of light to activate photosensitizing drugs that generate oxygen radicals, specifically targeting cancer cells.
AI-Powered Genomics Platform
The University of Queensland and Cambridge have developed DNAscent, an AI-powered genomics platform that combines artificial intelligence with nanopore DNA sequencing to study DNA replication in cancer cells. This technology enables more precise identification of biomarkers that predict tumor response to chemotherapy and measures replication stress—a key cancer characteristic.
Stanford's Synthetic Peptide Innovation
Stanford researchers have created a revolutionary synthetic peptide that mimics the p53 tumor suppressor protein, killing cancer cells from within while reducing side effects and resisting mutation. This ring-shaped molecule is more stable than linear alternatives and can survive in the body long enough to reach targets and remain functional.
Clinical Impact and Patient Outcomes
The real-world impact of these breakthroughs is already being felt in cancer centers worldwide. Dual-target CAR-T cell therapy for aggressive brain cancer (glioblastoma) has shown tumor shrinkage in nearly two-thirds of patients, with several living 12 months or longer—remarkable considering typical survival is less than a year.
For pancreatic cancer, historically one of the deadliest forms, researchers have identified new protein targets that could prevent tumors from becoming aggressive and spreading. This discovery offers hope for developing drugs that could keep patients living well for longer periods.
The Future of Cancer Treatment
These 2025 breakthroughs represent more than incremental improvements—they signal a fundamental transformation in how we approach cancer treatment. The shift toward precision medicine, AI-guided therapies, and smart immune cell engineering suggests we're entering an era where cancer may become a manageable chronic condition rather than a death sentence.
The convergence of ultrasound-controlled therapies, universal vaccines, and personalized medicine offers unprecedented opportunities for combination treatments tailored to individual patients. As these technologies mature and move through clinical trials, they promise to revolutionize cancer care, potentially making surgery, chemotherapy, and radiation therapy obsolete for many cancer types.
With over 28 FDA approvals for immunotherapy drugs already announced in 2025—12 of which are immunotherapy agents—we're witnessing the fastest pace of cancer treatment innovation in medical history. These breakthroughs don't just offer hope; they're actively saving lives and transforming cancer from a feared diagnosis into a treatable condition.
The battle against cancer has entered a new phase, armed with smart cells, universal vaccines, and precision targeting. For the millions of patients and families affected by cancer worldwide, 2025 may well be remembered as the year everything changed.



